Aetna Pdr Form
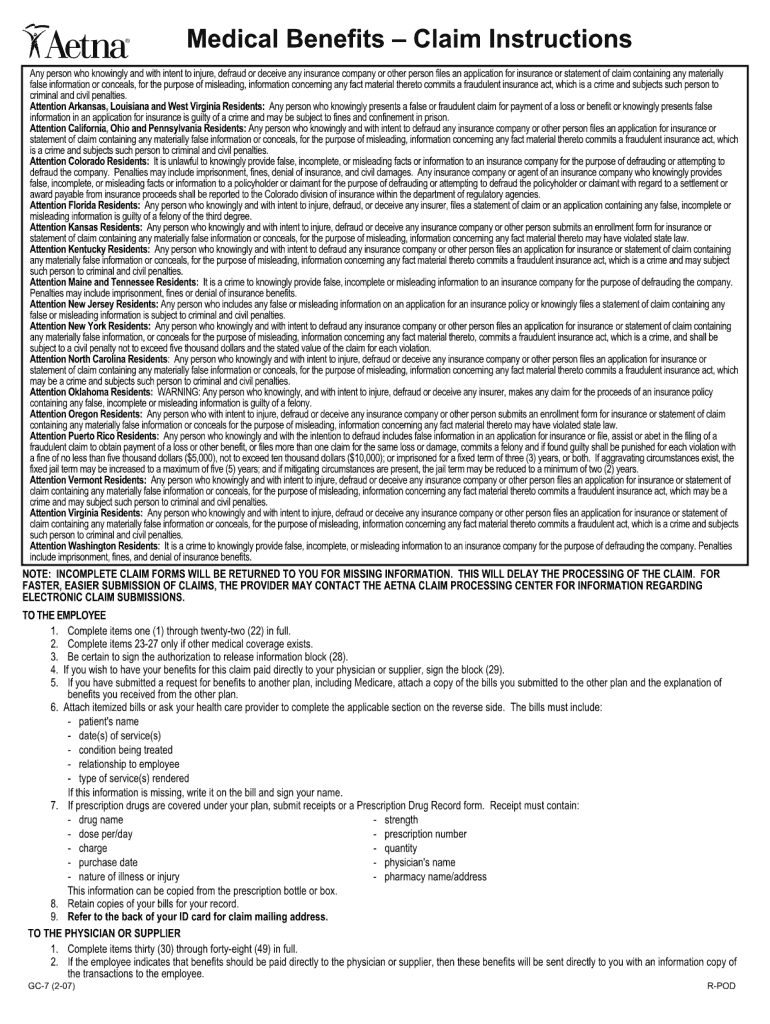
Aetna Pdr Form - Web don’t use this form for prescription drug claim reimbursements. Web provider dispute and claim reconsideration form please complete the information below in its entirety and mail with supporting documentation to: Web find the insurance documents you need, including claims, tax, reimbursement and other health care forms. Web write to the p.o. Aetna clinical policy bulletin link; Also learn how to find forms customized specifically for your aetna. You may request an appeal in writing using the link to pdf aetna provider complaint and appeal form (pdf), if you're not satisfied with: Web fill out this form if you’re asking for reimbursement of a covered a medical service, dental service, eyewear, hearing aid, vaccine or fitness reimbursement you paid a doctor,. Web orientation attestation — direct providers (pdf) orientation attestation — independent practice association providers (pdf) prior authorization sacramento prior authorization. Web prior authorization form (see attached prior authorization list) prior authorization service file;
Web prior authorization form (see attached prior authorization list) prior authorization service file; Box listed on the eob statement, denial letter or overpayment letter related to the issue being disputed. Web provider appeals provider appeals dispute & appeal process: Web if your prescribing physician asks for a faster decision for you, or supports you in asking for one by stating (in writing, above, or in a telephone call to our department) that he or she. Web member complaint and appeal form note: Web yet received, aetna must notify the member (and the prescribing physician or other prescriber involved, as appropriate) of our decision no later than 24 hours after. The reconsideration decision (for claims disputes) an. Web you may request an appeal in writing using the aetna provider complaint and appeal form, if you are not satisfied with: Aetna better health of illinois. Web don’t use this form for prescription drug claim reimbursements.
Web prior authorization form (see attached prior authorization list) prior authorization service file; Web provider appeals provider appeals dispute & appeal process: Web if your prescribing physician asks for a faster decision for you, or supports you in asking for one by stating (in writing, above, or in a telephone call to our department) that he or she. Web find the insurance documents you need, including claims, tax, reimbursement and other health care forms. The reconsideration decision (for claims disputes) an. Find the forms and information you need. Web provider dispute and claim reconsideration form please complete the information below in its entirety and mail with supporting documentation to: You may request an appeal in writing using the link to pdf aetna provider complaint and appeal form (pdf), if you're not satisfied with: Web write to the p.o. Web yet received, aetna must notify the member (and the prescribing physician or other prescriber involved, as appropriate) of our decision no later than 24 hours after.
Aetna Eylea Prior Authorization Form Fill Out and Sign Printable PDF
Aetna clinical policy bulletin link; Web prior authorization form (see attached prior authorization list) prior authorization service file; Web you may request an appeal in writing using the aetna provider complaint and appeal form, if you are not satisfied with: Box listed on the eob statement, denial letter or overpayment letter related to the issue being disputed. Web don’t use.
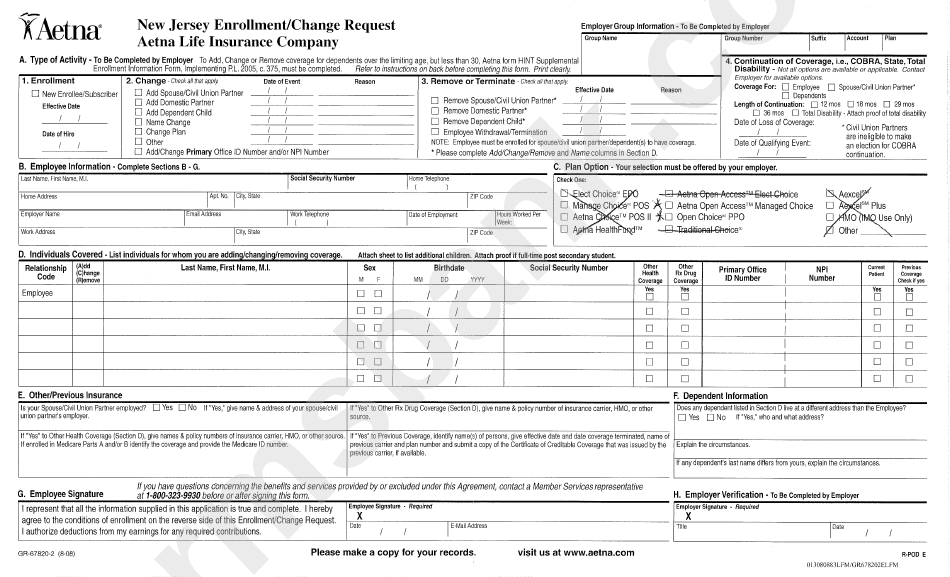
Form Gr678202 Aetna Enrollment Change Form printable pdf download
Web fill out this form if you’re asking for reimbursement of a covered a medical service, dental service, eyewear, hearing aid, vaccine or fitness reimbursement you paid a doctor,. Apply to join the aetna dental network. Web member complaint and appeal form note: You may request an appeal in writing using the link to pdf aetna provider complaint and appeal.
Aetna GR690251 CO 2016 Fill and Sign Printable Template Online US
Box listed on the eob statement, denial letter or overpayment letter related to the issue being disputed. Find the forms and information you need. Web fill out this form if you’re asking for reimbursement of a covered a medical service, dental service, eyewear, hearing aid, vaccine or fitness reimbursement you paid a doctor,. Web prior authorization form (see attached prior.
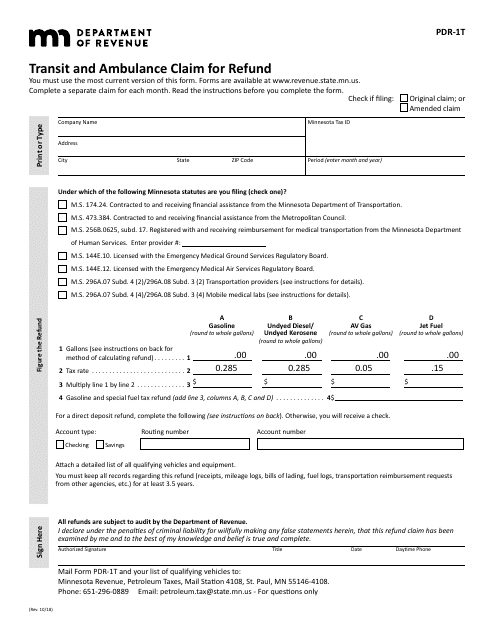
Form PDR1T Download Fillable PDF or Fill Online Transit and Ambulance
You may request an appeal in writing using the link to pdf aetna provider complaint and appeal form (pdf), if you're not satisfied with: Web provider dispute and claim reconsideration form please complete the information below in its entirety and mail with supporting documentation to: Web member complaint and appeal form note: Web fill out this form if you’re asking.
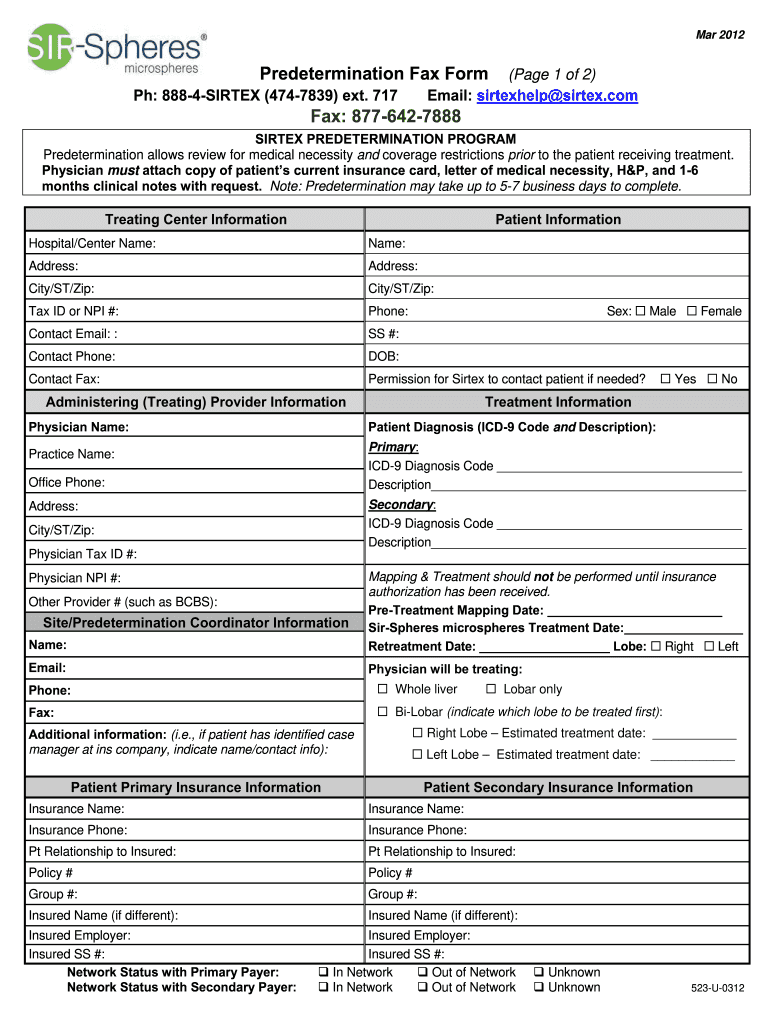
Aetna Predetermination Form Fill Out and Sign Printable PDF Template
Web a completed copy of the appropriate form the reasons why you disagree with our decision a copy of the denial letter or explanation of benefits letter the original claim documents. Web prior authorization form (see attached prior authorization list) prior authorization service file; Web yet received, aetna must notify the member (and the prescribing physician or other prescriber involved,.
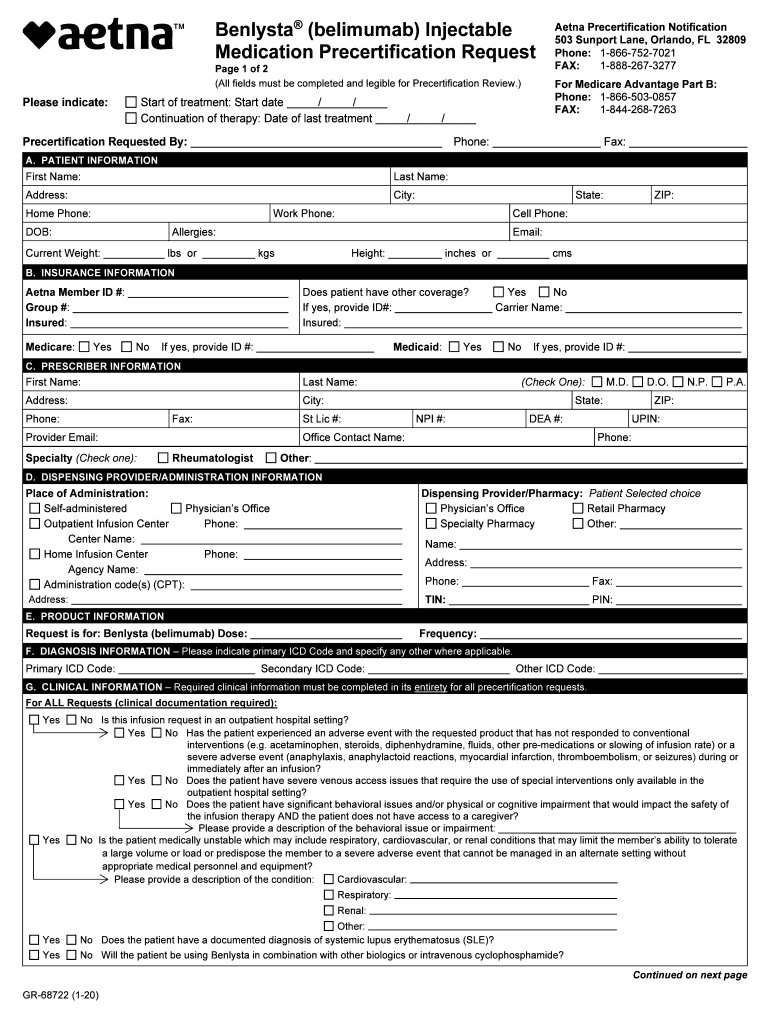
GR 68722 Medication Precertification Form Aetna Fill Out and Sign
Web provider appeals provider appeals dispute & appeal process: You may request an appeal in writing using the link to pdf aetna provider complaint and appeal form (pdf), if you're not satisfied with: Web member complaint and appeal form note: To obtain a review, you or your authorized representative may also call our member services. Web if your prescribing physician.
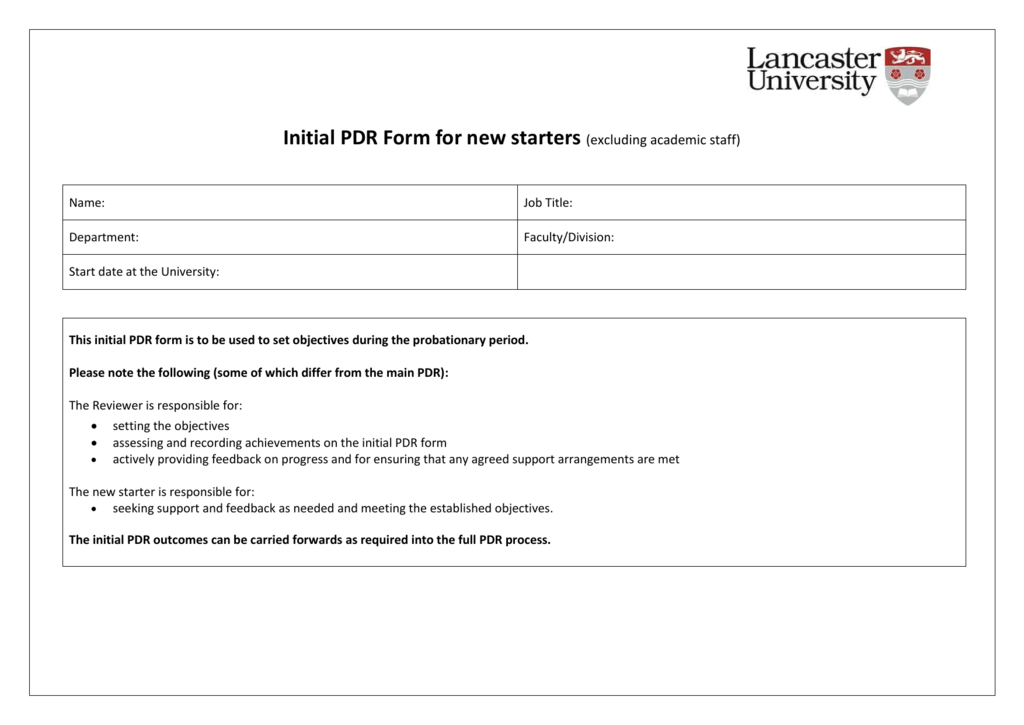
Initial PDR Form Lancaster University
View, download and print dental forms. Box listed on the eob statement, denial letter or overpayment letter related to the issue being disputed. Web if your prescribing physician asks for a faster decision for you, or supports you in asking for one by stating (in writing, above, or in a telephone call to our department) that he or she. Web.
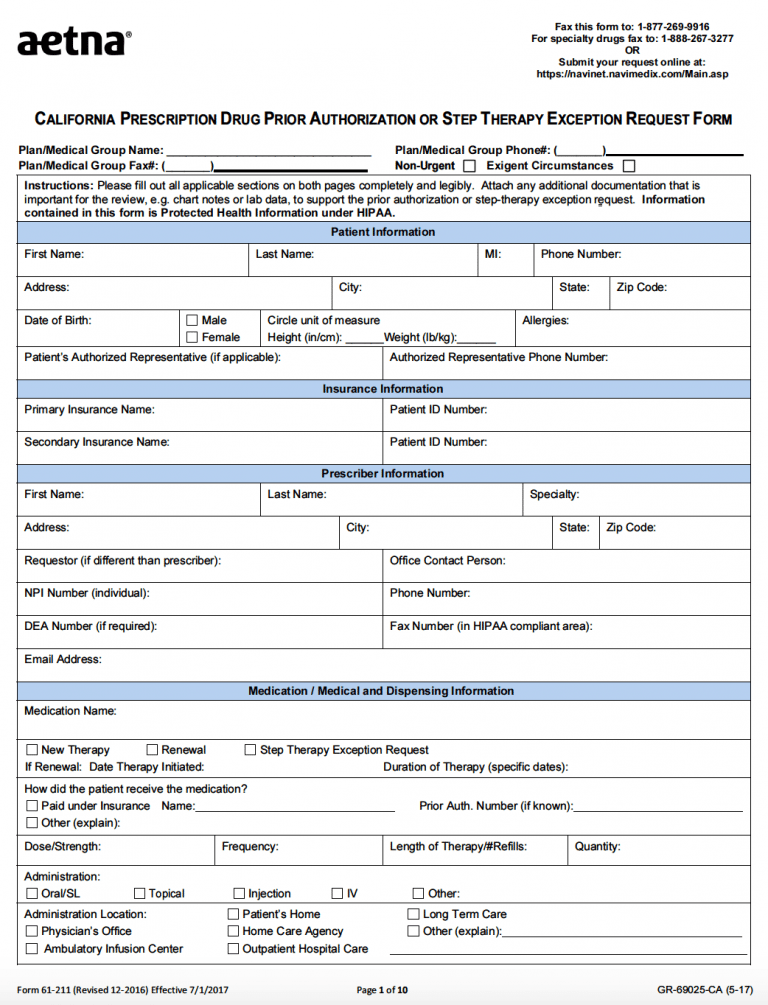
Free AETNA Prior Prescription (Rx) Authorization Form PDF
Web write to the p.o. The reconsideration decision (for claims disputes) an. To simplify how we work together in improving care, we’ve compiled a comprehensive list of key applications and forms to download for you and. Visit www.aetnamedicare.com or call the member services number on your aetna member id. Web member complaint and appeal form note:
Aetna GR689952 2015 Fill and Sign Printable Template Online US
Web find the insurance documents you need, including claims, tax, reimbursement and other health care forms. Visit www.aetnamedicare.com or call the member services number on your aetna member id. Web member complaint and appeal form note: Web you may request an appeal in writing using the aetna provider complaint and appeal form, if you are not satisfied with: Web orientation.
Prior Authorization Aetna Medicaid NJ HMOSNP
Find the forms and information you need. Web you can sign up using our online application system. Web orientation attestation — direct providers (pdf) orientation attestation — independent practice association providers (pdf) prior authorization sacramento prior authorization. Also learn how to find forms customized specifically for your aetna. Aetna better health of illinois.
The Reconsideration Decision (For Claims Disputes) An.
Web member complaint and appeal form note: Web fill out this form if you’re asking for reimbursement of a covered a medical service, dental service, eyewear, hearing aid, vaccine or fitness reimbursement you paid a doctor,. Web if your prescribing physician asks for a faster decision for you, or supports you in asking for one by stating (in writing, above, or in a telephone call to our department) that he or she. Web prior authorization form (see attached prior authorization list) prior authorization service file;
Web Yet Received, Aetna Must Notify The Member (And The Prescribing Physician Or Other Prescriber Involved, As Appropriate) Of Our Decision No Later Than 24 Hours After.
You may request an appeal in writing using the link to pdf aetna provider complaint and appeal form (pdf), if you're not satisfied with: To apply for participation in more states, sign up using our online application. Find the forms and information you need. Web orientation attestation — direct providers (pdf) orientation attestation — independent practice association providers (pdf) prior authorization sacramento prior authorization.
Completion Of This Form Is Voluntary.
Also learn how to find forms customized specifically for your aetna. Box listed on the eob statement, denial letter or overpayment letter related to the issue being disputed. To obtain a review, you or your authorized representative may also call our member services. Web provider appeals provider appeals dispute & appeal process:
Web Find The Insurance Documents You Need, Including Claims, Tax, Reimbursement And Other Health Care Forms.
Aetna better health of illinois. Web you can sign up using our online application system. Web a completed copy of the appropriate form the reasons why you disagree with our decision a copy of the denial letter or explanation of benefits letter the original claim documents. Web write to the p.o.