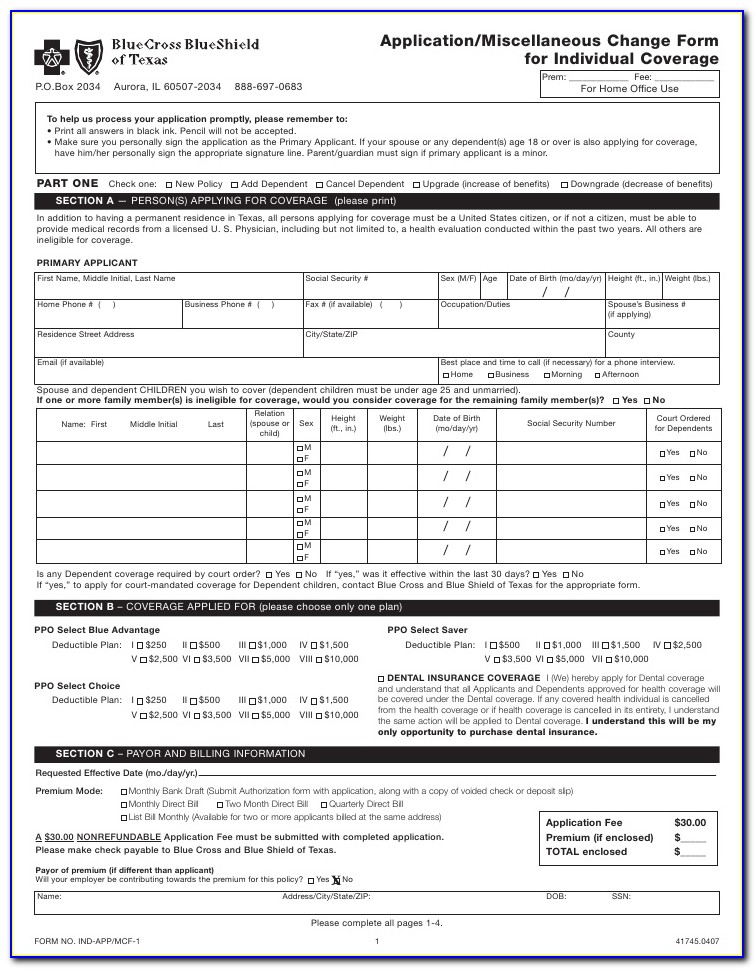
Ameriben Bcbs Prior Authorization Form
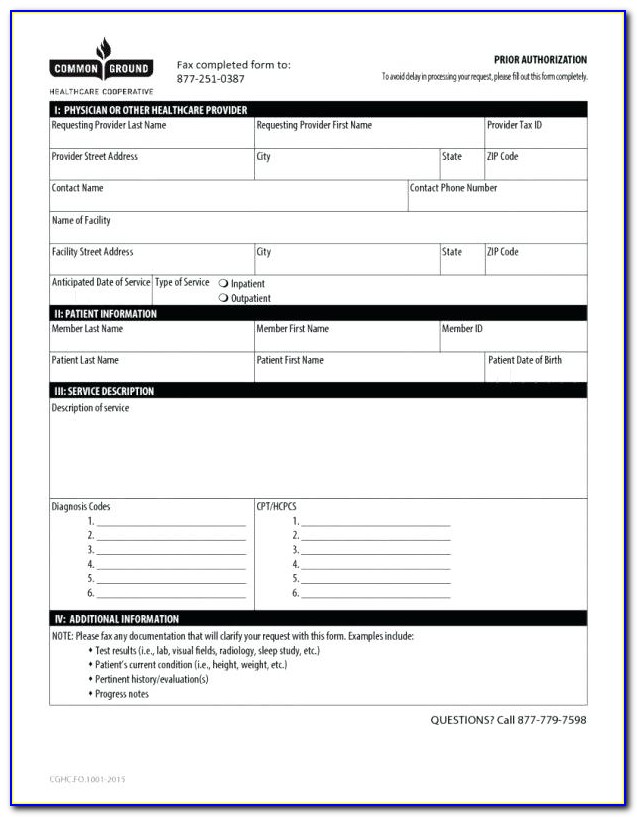
Ameriben Bcbs Prior Authorization Form - Please note that due to federal. Courtesy review form how to submit and view your authorizations. Web find out if prior authorization is required by entering the group number and procedure code. Web up to $40 cash back the ameriben prior authorization form is a document provided by ameriben that healthcare providers or patients can use to request prior authorization for a. Member’s ameriben id number 4. This will attach the patient’s name to the authorization and allow you to look at any previous authorizations you have created for this patient. Refer to your id card for the contact number. Web customize their prior authorization requirements. Web up to $40 cash back ameriben's prior authorization form requires the following information: Easily fill out pdf blank, edit, and sign them.
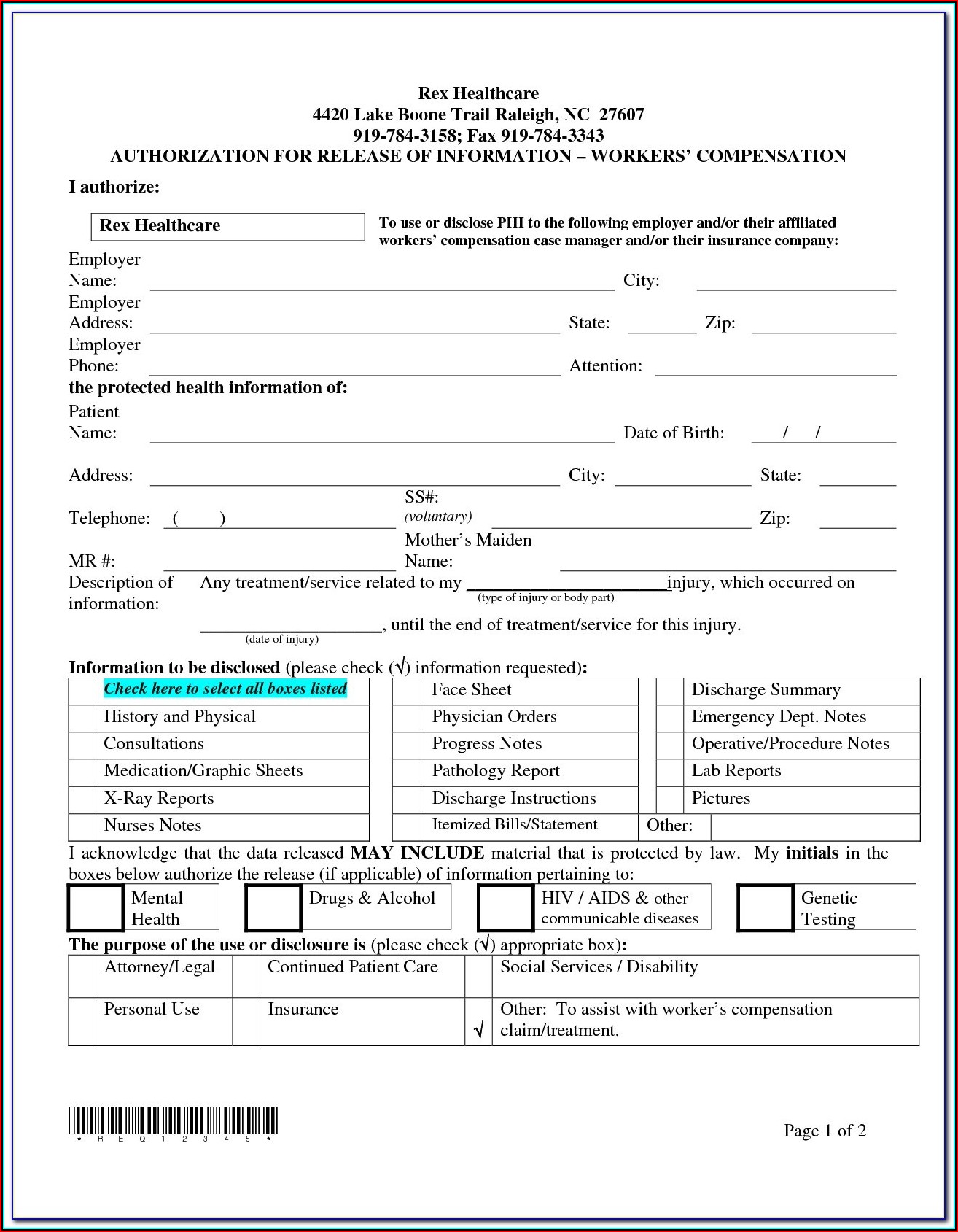
Web precertification fax request form personal & confidential urgent/ stat request(s) must be called into medical management: Employer group phone number fax number. Web for all myameriben log in issues, please email us at: Enjoy smart fillable fields and interactivity. Member’s date of birth 3. Save or instantly send your ready documents. Web i understand that as a result of this authorization, ameriben may disclose and release information concerning benefit eligibility, claim status, or claim approval or denial reasons. Please note that due to federal hipaa guidelines; Please note that due to federal. Web up to $40 cash back the ameriben prior authorization form is a document provided by ameriben that healthcare providers or patients can use to request prior authorization for a.
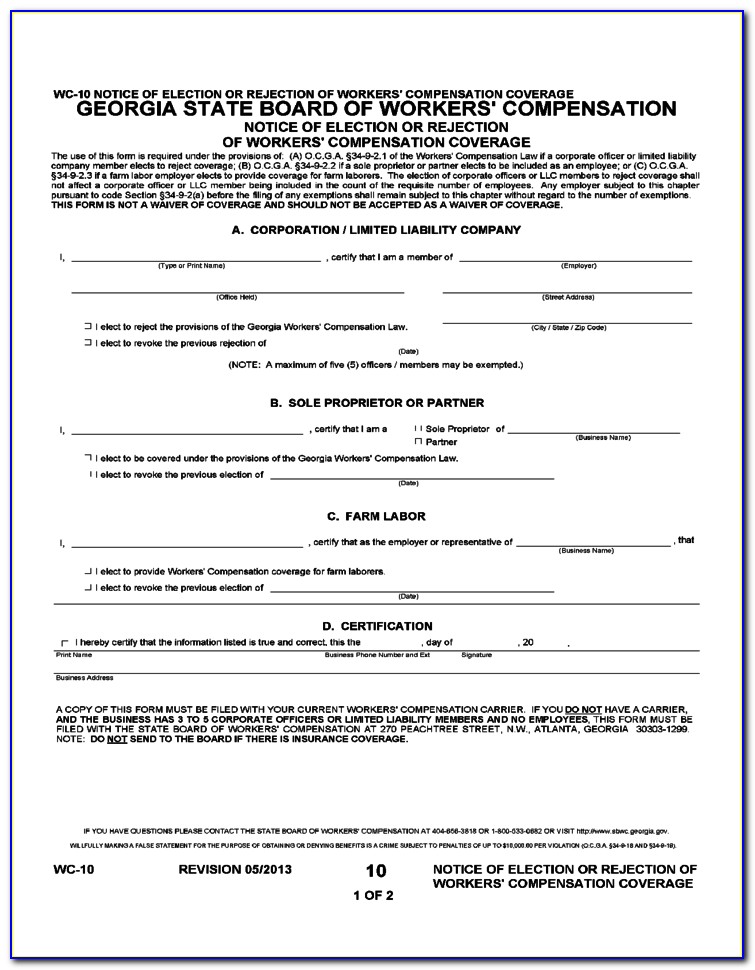
Please note that due to federal. Web for all myameriben log in issues, please email us at: Located online under “specialty pharmacy precertification” •. Web find out if prior authorization is required by entering the group number and procedure code. Web up to $40 cash back ameriben's prior authorization form requires the following information: Inpatient confinements (except hospice) for example, surgical and nonsurgical stays, stays in a skilled nursing facility or rehabilitation facility,. Web services that require precertification: Easily fill out pdf blank, edit, and sign them. Employer group phone number fax number. Web how to fill out and sign ameriben prior authorization form online?
Covermymeds Humana Prior Auth Form Form Resume Examples bX5aVMLOwW
Courtesy review form how to submit and view your authorizations. Refer to your id card for the contact number. Please note that due to federal hipaa guidelines; Enjoy smart fillable fields and interactivity. This will attach the patient’s name to the authorization and allow you to look at any previous authorizations you have created for this patient.
Aetna Medicare Advantage Disenrollment Form Form Resume Examples
Web how to request precertification/authorization mental health, substance abuse or behavioral health services require precertification/authorization. Employer group phone number fax number. Web prior authorization forms and templates prior authorization forms and templates download and print the most commonly requested prior authorization fax forms for. This will attach the patient’s name to the authorization and allow you to look at any.
Ach Payment Authorization Form Template Template 2 Resume Examples
Web i understand that as a result of this authorization, ameriben may disclose and release information concerning benefit eligibility, claim status, or claim approval or denial reasons. Web for all myameriben log in issues, please email us at: Web up to $40 cash back the ameriben prior authorization form is a document provided by ameriben that healthcare providers or patients.
Bcbs Prior Auth Forms Florida Form Resume Examples A4kn4J95jG
Member’s ameriben id number 4. Web prior authorization forms and templates prior authorization forms and templates download and print the most commonly requested prior authorization fax forms for. Courtesy review form how to submit and view your authorizations. Refer to your id card for the contact number. Web find out if prior authorization is required by entering the group number.
Bcbs Prior Authorization Form For Radiology Form Resume Examples
Web up to $40 cash back the ameriben prior authorization form is a document provided by ameriben that healthcare providers or patients can use to request prior authorization for a. Web up to $40 cash back ameriben's prior authorization form requires the following information: Easily fill out pdf blank, edit, and sign them. Please note that due to federal. Web.
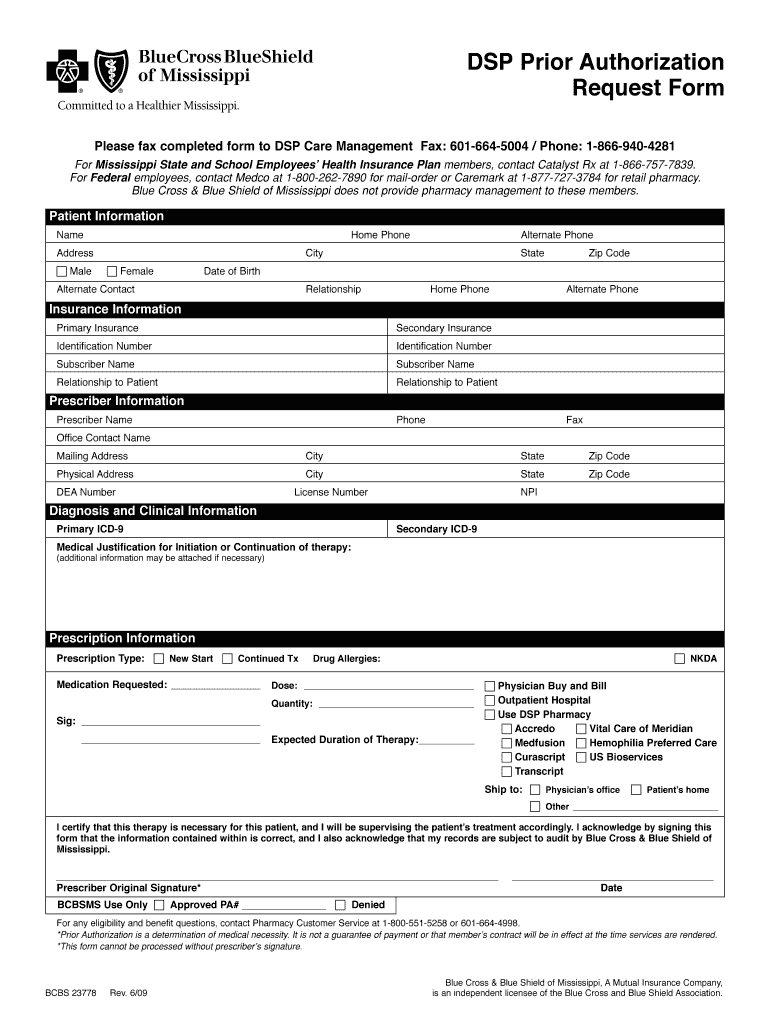
Bcbs Of Mississippi Prior Authorization Form Fill Online, Printable
Web i understand that as a result of this authorization, ameriben may disclose and release information concerning benefit eligibility, claim status, or claim approval or denial reasons. Web how to fill out and sign ameriben prior authorization form online? Web for all myameriben log in issues, please email us at: Use get form or simply click on the template preview.
Ameriben Precertification Form
You must submit an electronic. Web customize their prior authorization requirements. Web services that require precertification: Located online under “specialty pharmacy precertification” •. Employer group phone number fax number.
Bcbs Prior Auth Forms Florida Form Resume Examples A4kn4J95jG
Web up to $40 cash back the ameriben prior authorization form is a document provided by ameriben that healthcare providers or patients can use to request prior authorization for a. Employer group phone number fax number. Refer to your id card for the contact number. Please note that due to federal hipaa guidelines; Member’s date of birth 3.
Highmark Bcbs Medication Prior Authorization form Inspirational Billing
Web find out if prior authorization is required by entering the group number and procedure code. Web how to request precertification/authorization mental health, substance abuse or behavioral health services require precertification/authorization. Web i understand that as a result of this authorization, ameriben may disclose and release information concerning benefit eligibility, claim status, or claim approval or denial reasons. Web customize.
Bcbs Prior Authorization Form Maryland Form Resume Examples Yqlkmob5aj
Member’s date of birth 3. Member’s ameriben id number 4. Web precertification fax request form personal & confidential urgent/ stat request(s) must be called into medical management: Use get form or simply click on the template preview to open it in the editor. Web i understand that as a result of this authorization, ameriben may disclose and release information concerning.
Web Find Out If Prior Authorization Is Required By Entering The Group Number And Procedure Code.
Web up to $40 cash back the ameriben prior authorization form is a document provided by ameriben that healthcare providers or patients can use to request prior authorization for a. Please note that due to federal hipaa guidelines; Inpatient confinements (except hospice) for example, surgical and nonsurgical stays, stays in a skilled nursing facility or rehabilitation facility,. Refer to your id card for the contact number.
You Must Submit An Electronic.
Web precertification fax request form personal & confidential urgent/ stat request(s) must be called into medical management: Member’s ameriben id number 4. Save or instantly send your ready documents. Web customize their prior authorization requirements.
Please Note That Due To Federal.
Web how to request precertification/authorization mental health, substance abuse or behavioral health services require precertification/authorization. Web how to fill out and sign ameriben prior authorization form online? Employer group phone number fax number. Web up to $40 cash back ameriben's prior authorization form requires the following information:
Located Online Under “Specialty Pharmacy Precertification” •.
Web for all myameriben log in issues, please email us at: Courtesy review form how to submit and view your authorizations. Web i understand that as a result of this authorization, ameriben may disclose and release information concerning benefit eligibility, claim status, or claim approval or denial reasons. Member’s date of birth 3.