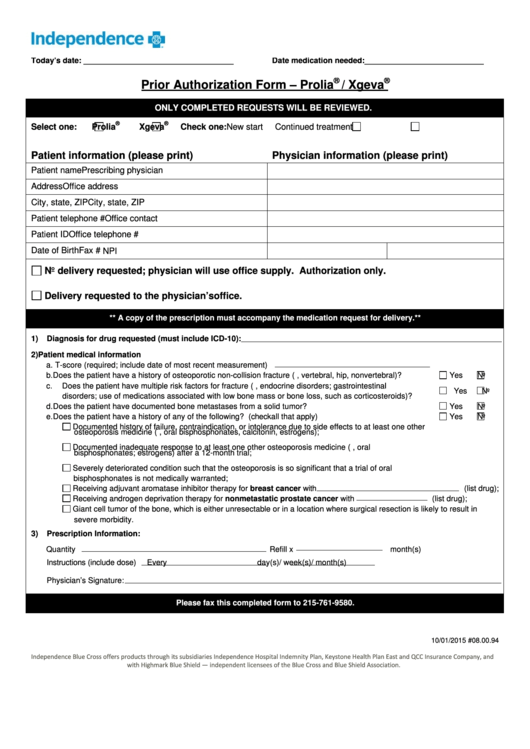
Bcbs Fep Pharmacy Prior Authorization Form
Bcbs Fep Pharmacy Prior Authorization Form - Web your health care provider can request prior approval electronically, by fax or by mail. Web prior authorization requests for drugs covered under the medical benefit must be submitted electronically through the carefirst provider portal. Web all forms must be signed, then either faxed or mailed. The full list of drugs that need to be approved, prior approval forms and additional information. Web the blue cross and blue shield service benefit plan has a variety of pharmacy programs to meet your prescription needs. Web blue cross and blue shield. Web most drugs are covered without requiring prior approval. Use the appropriate medication authorization request form below to request prior authorization for a medication that's covered under a member's. Web bcbsaz reserves the right to require prior authorization for such newly released and changed items even though the tool and code lists have not yet been updated to include. 6 23 23 norditropin noritate northera nourianz novarel noxafil nplate nubeqa nucala nucynta/nucytna er nuedexta numoisyn.
The full list of drugs that need to be approved, prior approval forms and additional information. Be the first to know about our benefits, wellness incentives and rewards you're eligible for with your plan. Web premera blue cross is an independent licensee of the blue cross blue shield association serving businesses and residents of alaska and washington state, excluding clark. Web all forms must be signed, then either faxed or mailed. Get access to over 55,000 retail pharmacies. Web to obtain a fax form, visit the prior authorization forms page. The increase in requests include an unusual number. Web 2023 fep prior approval drug list rev. Web get the latest from fep. 6 23 23 norditropin noritate northera nourianz novarel noxafil nplate nubeqa nucala nucynta/nucytna er nuedexta numoisyn.
Web select the appropriate fep form to get started. Web blue cross commercial forms. Web most drugs are covered without requiring prior approval. Web blue cross and blue shield. Get access to over 55,000 retail pharmacies. Covermymeds is fep prior authorization forms’s preferred method for receiving epa requests. Explore prior approval topics learn about prior. Web to obtain a fax form, visit the prior authorization forms page. Web this page provides prior approval requirements, contact information, and forms for the federal employee program (fep). Web premera blue cross is an independent licensee of the blue cross blue shield association serving businesses and residents of alaska and washington state, excluding clark.
Wellpoint Pharmacy Prior Authorization Forms PharmacyWalls
Web your health care provider can request prior approval electronically, by fax or by mail. The full list of drugs that need to be approved, prior approval forms and additional information. Web or call the number on the back of the member id card. Get access to over 55,000 retail pharmacies. Covermymeds is fep prior authorization forms’s preferred method for.
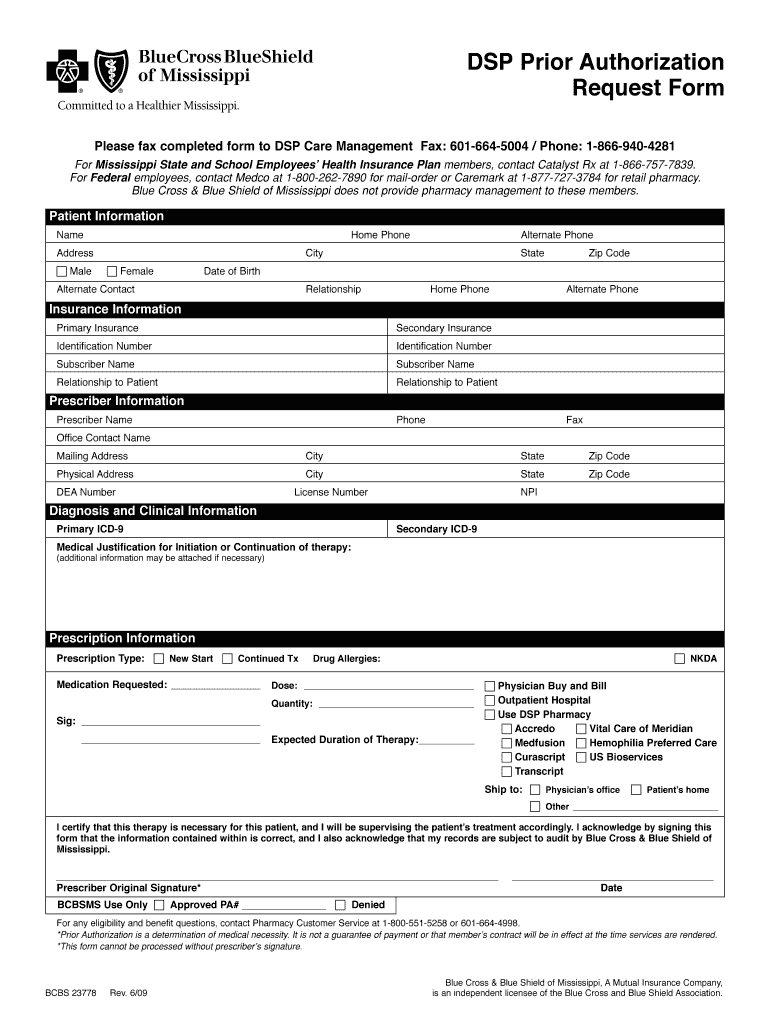
Bcbs Of Mississippi Prior Authorization Form Fill Online, Printable
Web federal employee program (fep) medical authorizations. Web • pharmacy nabp or npi number or the current name and complete address of pharmacy • full name of the patient • date filled • name of drug, strength (e.g., 500 mg) and. To submit a prior authorization. Covermymeds is fep prior authorization forms’s preferred method for receiving epa requests. Web director’s.
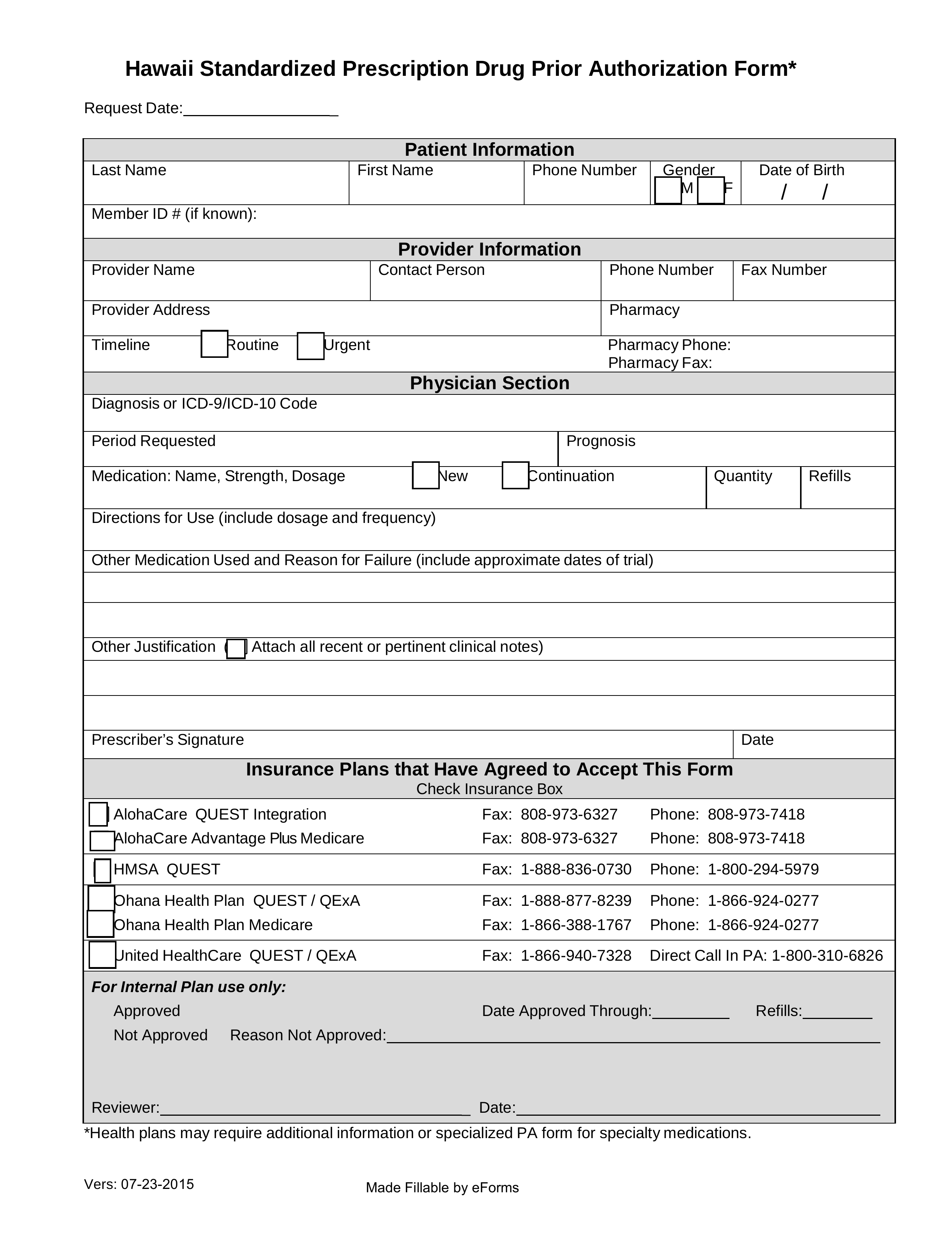
Free Hawaii Medicaid Prior (Rx) Authorization Form PDF eForms
Web view and download our medical, pharmacy and overseas claim forms. Web blue cross commercial forms. However, some select drugs require your doctor to provide information about your prescription to determine. Our employees are trained regarding the appropriate way to handle your private health information. Web bcbsaz reserves the right to require prior authorization for such newly released and changed.
Fep Prior Authorization Form â
Web prior authorization requests for drugs covered under the medical benefit must be submitted electronically through the carefirst provider portal. Get access to over 55,000 retail pharmacies. Web most drugs are covered without requiring prior approval. Explore prior approval topics learn about prior. Web the blue cross and blue shield service benefit plan has a variety of pharmacy programs to.
Bcbs Prior Authorization Form Ohio Form Resume Examples 9lV8N5A30o
Web to obtain a fax form, visit the prior authorization forms page. Web your health care provider can request prior approval electronically, by fax or by mail. Web the blue cross and blue shield service benefit plan has a variety of pharmacy programs to meet your prescription needs. For telephone contacts, please see the blue shield of california member authorizations.
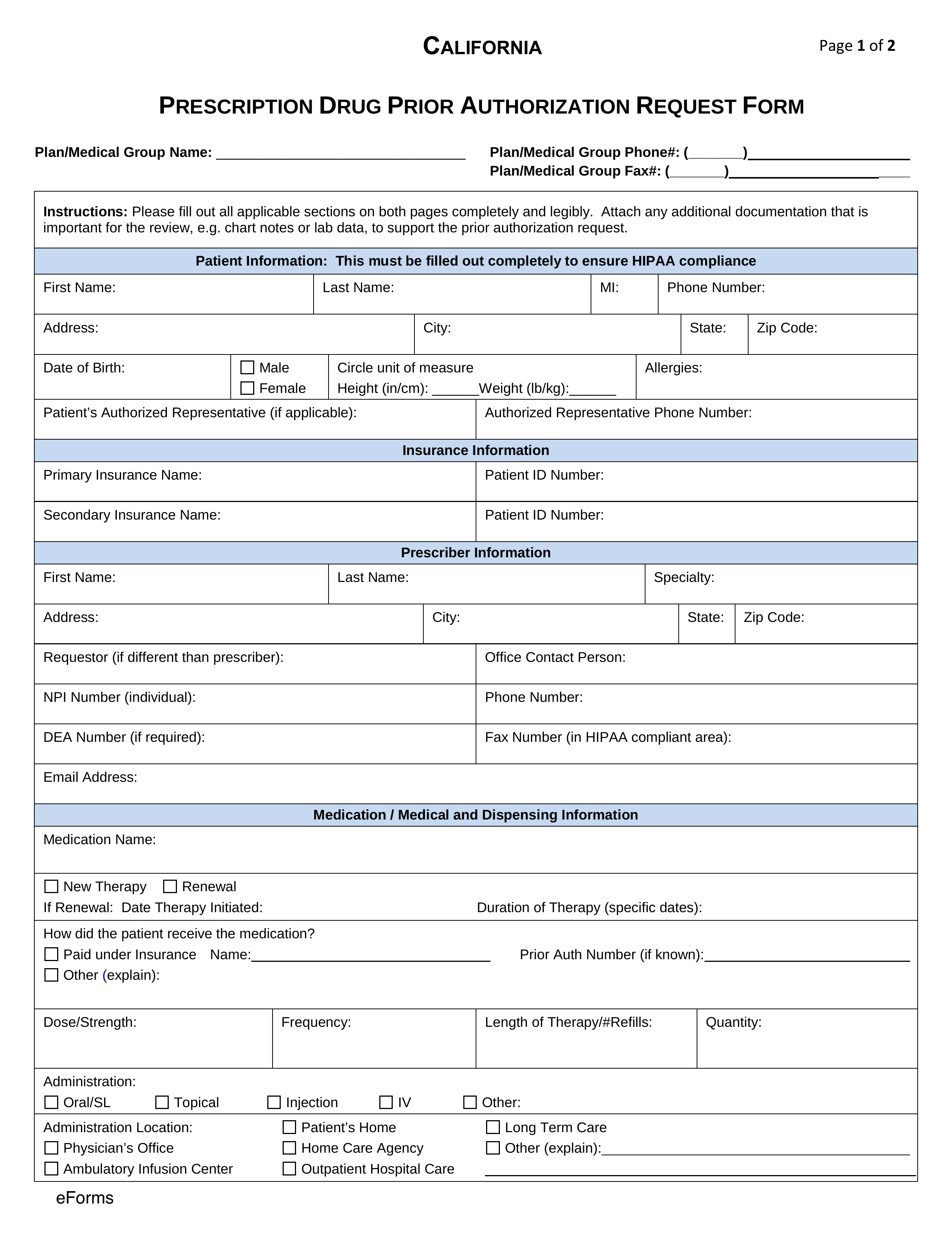
Free California Medicaid Prior (Rx) Authorization Form PDF eForms
Web the blue cross and blue shield service benefit plan has a variety of pharmacy programs to meet your prescription needs. Web get the latest from fep. Web 2023 fep prior approval drug list rev. However, some select drugs require your doctor to provide information about your prescription to determine. A prior approval, or pa, review determines medical necessity and.
42 Best Bcbs Nc Prior Authorization forms for
Explore prior approval topics learn about prior. Web get the latest from fep. Web director’s office and fep’s own independent pharmacy and therapeutics committee • the pa process is coordinated between cvs caremark and the mail service provider on. Web blue cross and blue shield. Web prior authorization requests for drugs covered under the medical benefit must be submitted electronically.
Bcbs Prior Authorization Form Maryland Form Resume Examples Yqlkmob5aj
Be the first to know about our benefits, wellness incentives and rewards you're eligible for with your plan. 6 23 23 norditropin noritate northera nourianz novarel noxafil nplate nubeqa nucala nucynta/nucytna er nuedexta numoisyn. Web bcbsaz reserves the right to require prior authorization for such newly released and changed items even though the tool and code lists have not yet.
Bcbs Prior Authorization Form Tennessee Form Resume Examples
Web to obtain a fax form, visit the prior authorization forms page. Web 2023 fep prior approval drug list rev. Service benefit plan prior approval p.o. Web your health care provider can request prior approval electronically, by fax or by mail. Be the first to know about our benefits, wellness incentives and rewards you're eligible for with your plan.
Highmark bcbs member claim form
Web to obtain a fax form, visit the prior authorization forms page. The full list of drugs that need to be approved, prior approval forms and additional information. Web blue cross and blue shield. Web all forms must be signed, then either faxed or mailed. The increase in requests include an unusual number.
Web Premera Blue Cross Is An Independent Licensee Of The Blue Cross Blue Shield Association Serving Businesses And Residents Of Alaska And Washington State, Excluding Clark.
Web federal employee program (fep) medical authorizations. Web for all other questions regarding the submission of your request, please contact cvs caremark: Web blue cross commercial forms. The increase in requests include an unusual number.
Web This Page Provides Prior Approval Requirements, Contact Information, And Forms For The Federal Employee Program (Fep).
A prior approval, or pa, review determines medical necessity and considers fep benefits before a treatment, procedure,. Covermymeds is fep prior authorization forms’s preferred method for receiving epa requests. We’ve recently been inundated with a huge increase in prior authorization (pa) requests. Web view and download our medical, pharmacy and overseas claim forms.
Use The Appropriate Medication Authorization Request Form Below To Request Prior Authorization For A Medication That's Covered Under A Member's.
Service benefit plan prior approval p.o. 6 23 23 norditropin noritate northera nourianz novarel noxafil nplate nubeqa nucala nucynta/nucytna er nuedexta numoisyn. Your privacy is important to us. For telephone contacts, please see the blue shield of california member authorizations section on the authorization.
Be The First To Know About Our Benefits, Wellness Incentives And Rewards You're Eligible For With Your Plan.
Web select the appropriate fep form to get started. Web prior authorization requests for drugs covered under the medical benefit must be submitted electronically through the carefirst provider portal. Web blue cross and blue shield. The full list of drugs that need to be approved, prior approval forms and additional information.