Soap Note Template Mental Health
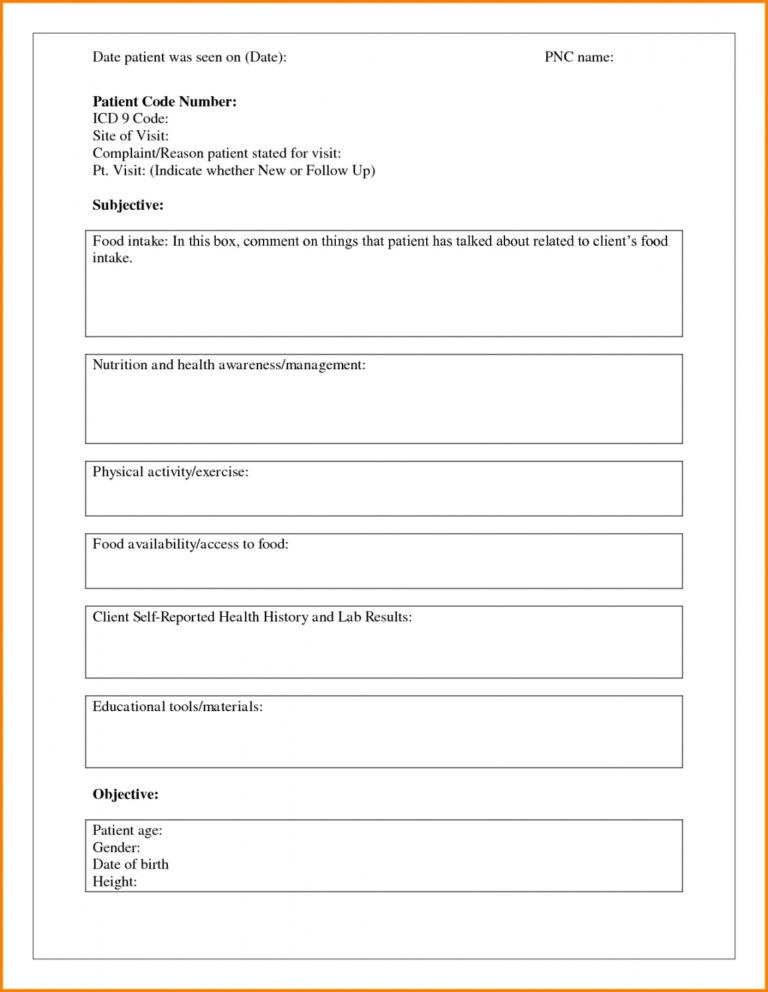
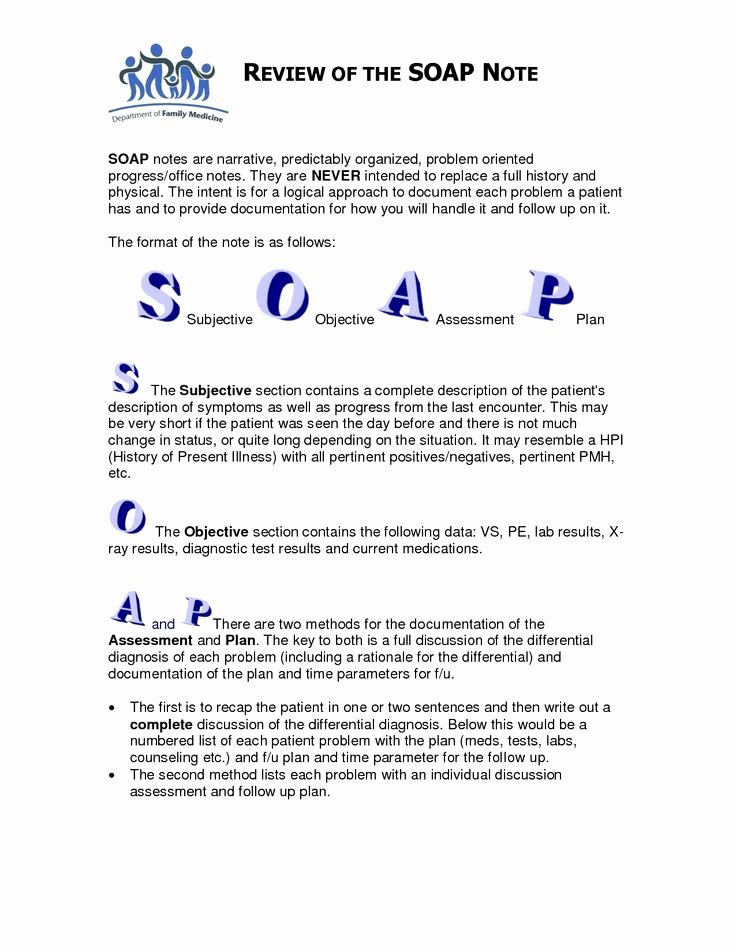
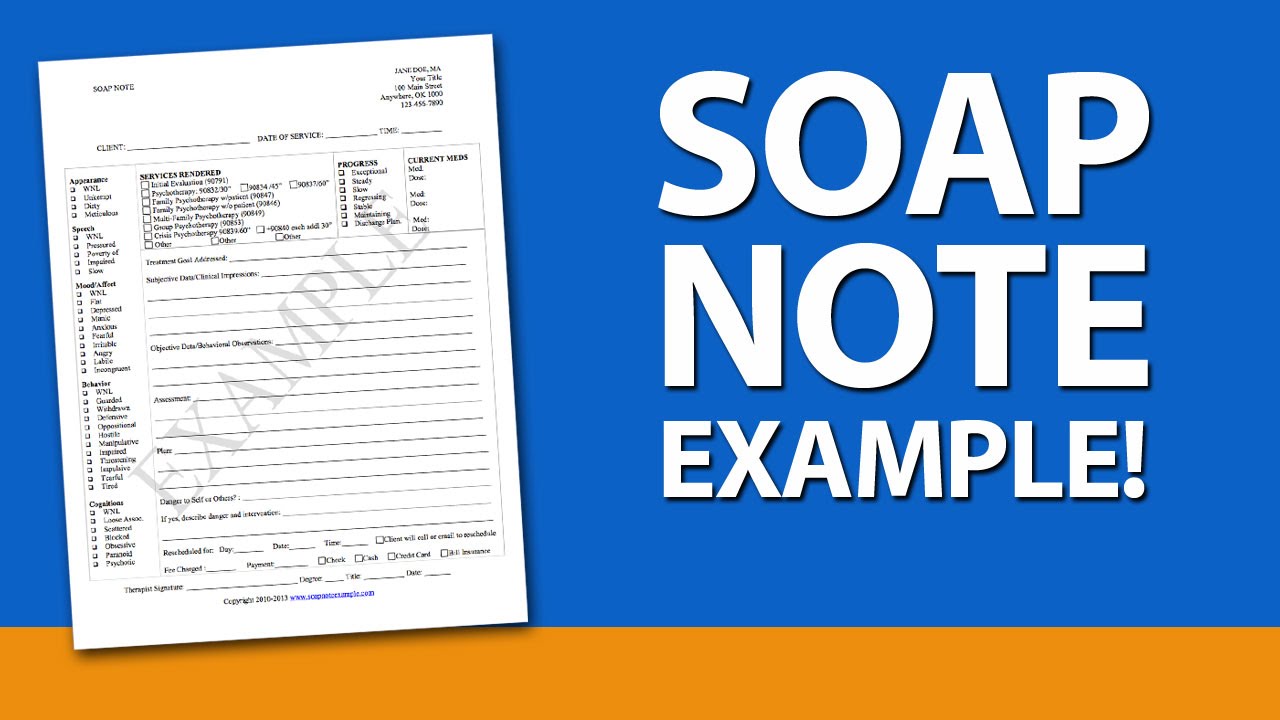
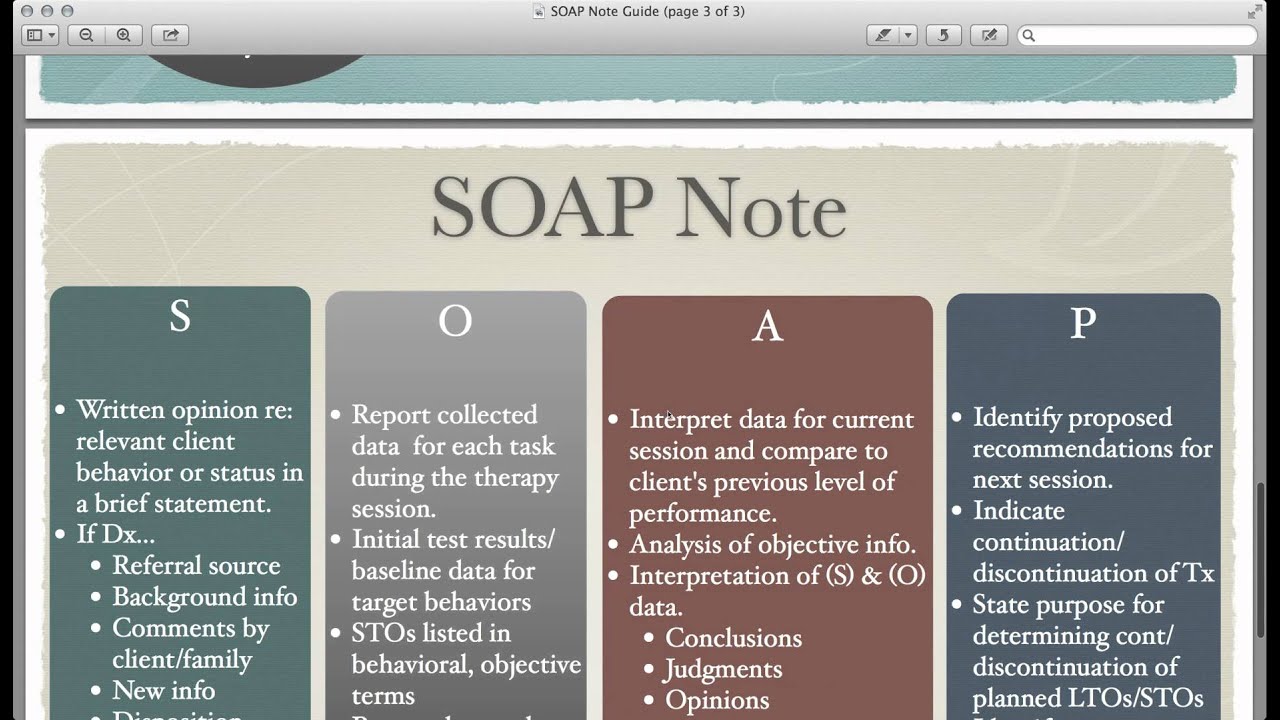
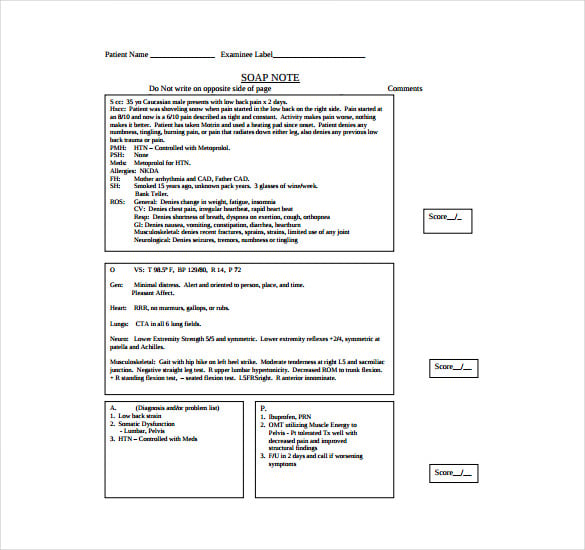
Soap Note Template Mental Health - Web subjective this covers your patient’s detailed medical history and current symptoms. This might include subjective information from a patient’s guardian or someone else involved in their care. S = subjective information, such as quotes from the client, or paraphrased statements they’ve given in session. Using a template such as soap note means that you can capture, store and interpret your client's information consistently, over time. Web introduction soap notes are a helpful method of documentation designed to assist medical professionals in streamlining their client notes. Download our comprehensive soap note pdf template for mental health professionals and other medical professionals for easy note taking and digital storage of client notes: Soap notes are the most common type, containing four separate types of information in four distinct rows:. To help streamline your clinical documentation process, we’ve created a reusable soap template: Record your patient’s chief complaint, existing symptoms, and any pain description in this section. Web soap notes pdf template for mental health providers.
Using a template such as soap note means that you can capture, store and interpret your client's information consistently, over time. Web life 30 blank soap note templates (+examples) march 28, 2021 9 mins read as a health care provider, the records you take decide the level of care that your patients experience. Soap note for medical practitioners (care cloud, n.d.): Health professionals must provide notes that are detailed, succinct, thorough, and simple for other practitioners to use. It’s best to choose a few sentences that best represent the most pressing concern your client brought into the session. Download our soap notes template pdf file right now. Web soap notes pdf template for mental health providers. Download our comprehensive soap note pdf template for mental health professionals and other medical professionals for easy note taking and digital storage of client notes: Here are three templates you can use for a medical visit, therapy, or coaching session. Web subjective this covers your patient’s detailed medical history and current symptoms.
Soap notes are the most common type, containing four separate types of information in four distinct rows:. It’s best to choose a few sentences that best represent the most pressing concern your client brought into the session. Notes from your verbal interaction with patients as well as what they tell you about their condition go here. A handful of commonly used abbreviations are included in the short note. Web soap notes pdf template for mental health providers. Health professionals must provide notes that are detailed, succinct, thorough, and simple for other practitioners to use. How to create effective medical progress notes according to the soap format. Download our soap notes template pdf file right now. Here are three templates you can use for a medical visit, therapy, or coaching session. Both meet minimum documentation standards and are acceptable for use.
Progress Note Template For Mental Health Counselors Template Business
Web subjective this covers your patient’s detailed medical history and current symptoms. How to create effective medical progress notes according to the soap format. Web life 30 blank soap note templates (+examples) march 28, 2021 9 mins read as a health care provider, the records you take decide the level of care that your patients experience. Record your patient’s chief.
Printable Soap Note Template Mental Health Heart Rate Zones Mental
To help streamline your clinical documentation process, we’ve created a reusable soap template: Web in this post, we will review what soap notes are, how to write a soap note, tips for effective soap notes, and a template you can use for your soap notes. Health professionals must provide notes that are detailed, succinct, thorough, and simple for other practitioners.
Psychiatric soap Note Example Peterainsworth
To help streamline your clinical documentation process, we’ve created a reusable soap template: Notes from your verbal interaction with patients as well as what they tell you about their condition go here. Carepatron’s downloadable soap template for medical progress notes. Record your patient’s chief complaint, existing symptoms, and any pain description in this section. Both meet minimum documentation standards and.
Soap Note Examples for Mental Health Counselors YouTube
It’s best to choose a few sentences that best represent the most pressing concern your client brought into the session. Record your patient’s chief complaint, existing symptoms, and any pain description in this section. Here are three templates you can use for a medical visit, therapy, or coaching session. Web introduction soap notes are a helpful method of documentation designed.
7 Best Images Of Printable Counseling Soap Note Templates in 2021
Web subjective this covers your patient’s detailed medical history and current symptoms. A handful of commonly used abbreviations are included in the short note. Download our comprehensive soap note pdf template for mental health professionals and other medical professionals for easy note taking and digital storage of client notes: Using a template such as soap note means that you can.
Pin on Products I Love
This might include subjective information from a patient’s guardian or someone else involved in their care. Download our soap notes template pdf file right now. Web the s.o.a.p acronym soap is an acronym for the 4 sections, or headings, that each progress note contains: Both meet minimum documentation standards and are acceptable for use. Web soap notes pdf template for.
Soap Notes Mental Health Template Great Professional Template
Record your patient’s chief complaint, existing symptoms, and any pain description in this section. Notes from your verbal interaction with patients as well as what they tell you about their condition go here. Here are three templates you can use for a medical visit, therapy, or coaching session. Please be mindful of these and use sparingly. This might include subjective.
Template‐ノートYouTube JapaneseClass.jp
This might include subjective information from a patient’s guardian or someone else involved in their care. Notes from your verbal interaction with patients as well as what they tell you about their condition go here. Please be mindful of these and use sparingly. Using a template such as soap note means that you can capture, store and interpret your client's.
Soap Note Template 9+ Free Word, PDF Format Download! Free
Please be mindful of these and use sparingly. Carepatron’s downloadable soap template for medical progress notes. It’s best to choose a few sentences that best represent the most pressing concern your client brought into the session. Web the s.o.a.p acronym soap is an acronym for the 4 sections, or headings, that each progress note contains: Using a template such as.
SOAP Notes PDF Template and Guide for Mental Health Providers
Record your patient’s chief complaint, existing symptoms, and any pain description in this section. Web soap notes pdf template for mental health providers. Web the s.o.a.p acronym soap is an acronym for the 4 sections, or headings, that each progress note contains: Web subjective this covers your patient’s detailed medical history and current symptoms. Carepatron’s downloadable soap template for medical.
A Handful Of Commonly Used Abbreviations Are Included In The Short Note.
Web subjective this covers your patient’s detailed medical history and current symptoms. Web soap notes pdf template for mental health providers. Health professionals must provide notes that are detailed, succinct, thorough, and simple for other practitioners to use. How to create effective medical progress notes according to the soap format.
Web In This Post, We Will Review What Soap Notes Are, How To Write A Soap Note, Tips For Effective Soap Notes, And A Template You Can Use For Your Soap Notes.
Notes from your verbal interaction with patients as well as what they tell you about their condition go here. Web introduction soap notes are a helpful method of documentation designed to assist medical professionals in streamlining their client notes. Record your patient’s chief complaint, existing symptoms, and any pain description in this section. Soap notes are the most common type, containing four separate types of information in four distinct rows:.
Web Life 30 Blank Soap Note Templates (+Examples) March 28, 2021 9 Mins Read As A Health Care Provider, The Records You Take Decide The Level Of Care That Your Patients Experience.
It’s best to choose a few sentences that best represent the most pressing concern your client brought into the session. Soap note for medical practitioners (care cloud, n.d.): Where a client’s subjective experiences, feelings, or perspectives are recorded. Carepatron’s downloadable soap template for medical progress notes.
Download Our Comprehensive Soap Note Pdf Template For Mental Health Professionals And Other Medical Professionals For Easy Note Taking And Digital Storage Of Client Notes:
S = subjective information, such as quotes from the client, or paraphrased statements they’ve given in session. Download our soap notes template pdf file right now. This might include subjective information from a patient’s guardian or someone else involved in their care. Please be mindful of these and use sparingly.